The arrival of the Covid-19 pandemic has had a significant impact on the lives of the entire world population, but if we also consider the impact on people affected by different chronic diseases, such as Alzheimer’s, Parkinson’s disease (PD), or cardiovascular pathologies, the scope is even greater.
Patients with Parkinson’s, Alzheimer’s, and cardiovascular disease are some of the most vulnerable to the virus due to their advanced age (in many cases) and underlying health conditions. This means they are more likely to experience severe symptoms if they contract Covid-19. But even without becoming infected with the virus or suffering mild symptoms, the patterns of self-isolation and social distancing, as well as other preventative measures that have become standard procedure throughout this pandemic, have led to a significant decline in their quality of life.
Furthermore, there has been an impact on physical well-being, closely related to confinement and being forced to stay indoors. Many people have reduced their activity levels due to various restrictions and out of fear of contracting the virus. This has led to weight gain in some individuals and a general worsening of their physical condition, resulting in increased physical symptoms such as muscle problems, aches and pains, increased stiffness, worsening gait, and reduced tolerance to exertion, among others.
In addition, higher levels of anxiety and stress related to the uncertainty of the situation, fear, and social isolation, have been observed. Covid-19 has negatively affected psychological well-being, with significant increases in cases of depression and low self-esteem. In addition, isolation from friends and family can lead to feelings of loneliness that may worsen depression or anxiety disorders.
In relation to this situation, the Spanish Parkinson’s Federation (FEP) analysed the impact of the pandemic on people with PD and their caregivers. The study revealed that the mobility of most people with PD worsened during the pandemic, which in turn correlated “strongly with poorer emotional well-being.” In addition, 67% of people with PD experienced losses in personal autonomy and independence, as they needed more help to carry out daily activities. Meanwhile, 31% of people with PD stopped rehabilitation therapies, often due to the inability to attend face-to-face sessions (Federación Española de Párkinson, 2021). These impacts contributed to the worsening quality of life that most people with PD experienced during the pandemic.
Consistent with the Spanish Parkinson’s Federation, Shalash et al. found that PD patients had worse stress, depression, anxiety, physical condition, and quality of life compared to control patients during the COVID-19 pandemic (Shalash et al., 2020). In addition, Kasar and Karaman found that older adults‘ loneliness and QoL were negatively affected during the pandemic, including older adults living in social service institutions, where many older patients reside (Kasar and Karaman, 2021). It is therefore important to recognise that the overall QoL of older populations worldwide worsened with the COVID-19 pandemic and to understand how this affects existing treatment tools.
The effects of the COVID-19 pandemic have reached all populations, each in a different way. However, the elderly and chronically ill have particularly felt the impacts of the pandemic. It is therefore essential that these effects are taken into account in the continuum of care, as well as in the development of new treatments and solutions. Healthcare institutions must strive to develop technologies that treat patients in new and innovative ways in response to the changing situation in the world. Digital tools and technologies, in particular, have great potential to create new treatment formats.
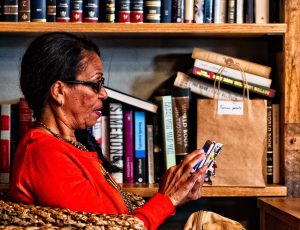
Jennifer Jiménez Ramos
Head the Innovation and Research Unit, Asociación Parkinson Madrid