Empowering citizen participation and facilitating the transformation of health and care services towards more digitised, person-centred, and community-based models of care are a challenge for the World Health Organization (WHO). The 2030 Agenda for Sustainable Development[1] highlights that the spread of information and communications technologies and global interconnectedness has the potential to accelerate human progress, bridge the digital divide, and develop knowledge societies.
Digital technologies are essential components of sustainable health systems and universal health coverage. To realise their potential, digital health initiatives must centre around the wider health needs of the population and be integrated into the digital health ecosystem. These initiatives should also be guided by a robust strategy that integrates leadership, financial, organisational, human and technological resources, and is used as the basis for a costed action plan which enables coordination among multiple stakeholders. The strategic approach should be able to work across multiple health priorities underpinned by standards and an architecture that enables this integration.[2]
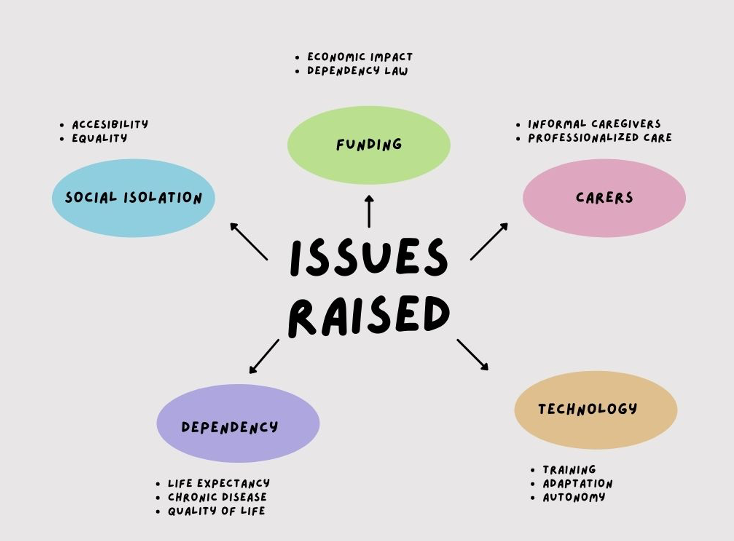
According to World Health Organization, most people prefer to live, and if possible spend their final days, at home. However, public policy has been slow to support a shift from institutions and hospitals to home-based settings. In all European countries, informal care accounts for the majority of care hours, even in countries with the largest publicly supported elderly care sectors. Nevertheless, most public funding for long-term care continues to go to institutional care: over 70% in Belgium, Iceland, and Switzerland. Such funding accounts for 0.3–3.9% of a country’s gross domestic product.
With the group aged ≥80 growing faster than any other and the average age of caregivers for the elderly rising, a better balance is needed between informal care and public support.
With regards to social care, sadly, there are older adults who are not able to participate in social activities. These people suffer from the effects of social isolation, which have an impact on their health status in terms of self-care management, adherence to treatment, and mental health, among others.
Social isolation is caused by various factors, such as physical weakness, physical disorders, mental illness, deterioration of psychological function, and social loss, among others. Senior isolation is becoming a major social problem in western countries. Many elderly people are living in single-resident homes without family or social support. Even in nursing homes, residents stay in their private bedrooms alone without participating in social activities. Since social isolation leads to serious consequences such as disuse syndrome, mental depression, suicide, etc., maintaining a person’s sense of community is very important.
[1] Adopted in United Nations General Assembly resolution 70/1 (2015)
[2] World Health Organization. Global Strategy on Digital Health. 2020. doi:10.1007/s13312-020-1789-7
Social impact: TeNDER's contribution
Our partners aim to understand and to help address some of the sources of social isolation in such settings. To this end, different health institutions from Spain (Servicio Madrileño de Salud (SERMAS), Asociación Parkinson Madrid (APM)); Germany (Schön Klinik Bad Aibling (SKBA)) and Slovenia (Spominčica Alzheimer Slovenija (SPO)) have developed and implemented an approach to study the social impact of the TeNDER system. We have interviewed key stakeholders, such as local authorities, health Professionals, and carers & associations.





